You are not alone if the new running season’s promise has encouraged your promise to develop healthier habits and increased activity. You may have started a walking or running program, joined a gym, or even resumed a sport that once brought great enjoyment. The benefits can be immeasurable — physically, emotionally, and mentally.
By now, however, you may also have discovered setbacks in the form of injury that can become costly, time-consuming, and discouraging.
As a podiatrist, one of the most common overuse injuries I see is heel pain after beginning a new exercise program. The individual is often interested in weight loss and has begun a walking or running program. The first few weeks go well, and they feel more energetic. Encouraged, they increase their exercise frequency, distance, and/or speed. Be careful! Too much too soon can lead to a gradual onset of pain in the bottom of one or both heels. The discomfort grows from a dull ache to a sharp stabbing pain. It’s usually worse with the first step in the morning or standing up after several minutes of sitting, then resolves (somewhat) with five to ten minutes of walking. Sometimes, the pain can be so severe it affects the ability to work.
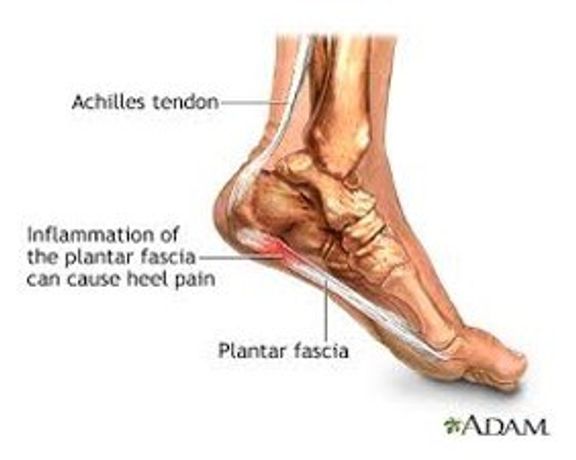
The plantar fascia is a ligament on the bottom of the foot that extends from the heel to the forefoot, almost to the toes. It serves as a thick covering to the four layers of muscles on the bottom of the foot and is a continuation of the Achilles tendon. The Achilles tendon resides in the back of the leg and flows continuously from its insertions above and below the knee to the back of the heel. When micro-tears develop in the plantar fascia at its origin under the heel, inflammation results, and plantar fasciitis begins. With chronic plantar fasciitis, the body begins reinforcing this weakened area with calcium, and a heel spur can become visible on X‑rays.
Etiology: What causes plantar fasciitis?
Factors contributing to plantar fasciitis can be intrinsic or extrinsic:
Intrinsic Anatomical considerations–
Flat feet, hypermobility in the joints, high arches, knock-knees (genu valgum) or bow-legs (genu varum), a tight Achilles tendon (equinus).
Extrinsic Considerations–
Inappropriate shoes that are worn out, with poor motion control, too much cushion, or inadequate arch support. Extrinsic considerations also include training schedules that increase intensity or duration too rapidly.
Treatment: What you can do:
Even Sun Tzu agrees that avoidance is the best strategy for overcoming any battle. Many great sources for training schedules are available to both beginning and advanced athletes. Select your program in advance, listen to your body, and give yourself permission to rest if needed. Remember that injury can be one of the greatest setbacks to your training goals. In the event of heel pain onset:
Rest: Substitution with cross-training in the form of swimming, bicycling — stationary or outside — circuit weight training and elliptical training may offer a viable substitute in the short run. However, complete rest from exercise may be required. For some, this may mean six weeks of an altered schedule before morning pain subsides. If this is successful, gradually return to normal impact activity, such as running, walking, or both.
Support: With a rigorous training schedule, be sure to replace running shoes every six months. Running/walking shoes are also designed with the intended purpose of stabilization, motion control, trail running, cushioning, etc. Be sure your shoes are in the appropriate condition and designed for your type of foot. You may also find that over-the-counter arch supports help.
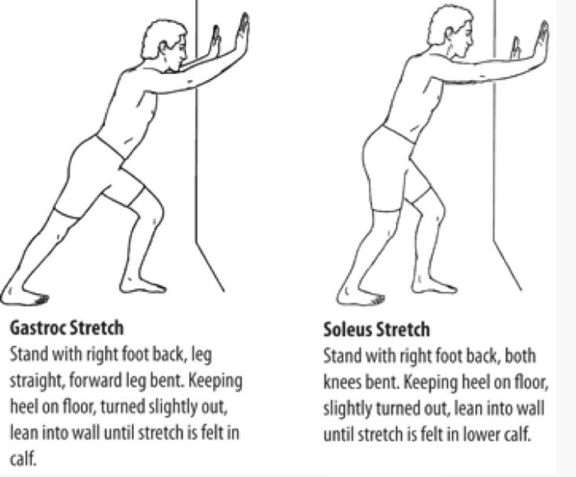
Stretching: The root cause behind most heel pain is a tight Achilles tendon complex. The “runner’s stretch” performed with the knee straight and knee bent will mobilize both muscles, contributing to this complex. You should target stretching each leg three times a day for a continuous minute with each stretch. This will allow your foot to properly load with each step and decrease the tendency toward hyper pronation.
What your doctor can do:
Your podiatrist can determine the underlying cause of your heel pain and develop a strategy for resolving it. This may include anti-inflammatories, physical therapy, a steroid injection, and/or custom orthotics. Most biomechanically caused heel pain can resolve with conservative treatment; however, in some cases, surgery may be required.
May your year be blessed with good health.
Dr. Kline is a board-certified podiatrist specializing in injury, wounds, and diseases of the foot and lower extremity.
Health Topics: